You're barely a few thrusts in when it happens again. That sharp, rising edge you’ve tried to breathe through, distract from, or delay is already taking over. You tense, try to hold back, and hope this time will be different. But it isn’t. Once more, you’ve climaxed far sooner than you wanted too.
The moment leaves you feeling defeated and disconnected, both from your partner and from yourself.
Premature ejaculation (PE) can feel like your body is working against you: uncooperative, difficult to manage, and deeply frustrating. And without a definitive cure, many individuals are left cycling through trial-and-error treatments that don’t fully deliver.
But a new wave of tech-based treatments is on the horizon, offering a potential drug-free, on-demand alternative. A 2024 study in IJIR: Your Sexual Medicine Journal reviews preliminary research on how they may help those grappling with PE delay ejaculation.
Although more in-depth studies are needed, the findings provide hope for improving quality of life and regaining a sense of control in the bedroom. 
What is premature ejaculation?
Recent research suggests 5% of men struggle with premature ejaculation.
The International Society for Sexual Medicine (ISSM) defines premature ejaculation based on three criteria:
1. Ejaculation happens very quickly after vaginal penetration.
2. There is a consistent inability to delay ejaculation during most or all sexual encounters involving vaginal penetration.
3. The experience leads to personal distress, frustration, or avoidance of sexual intimacy.
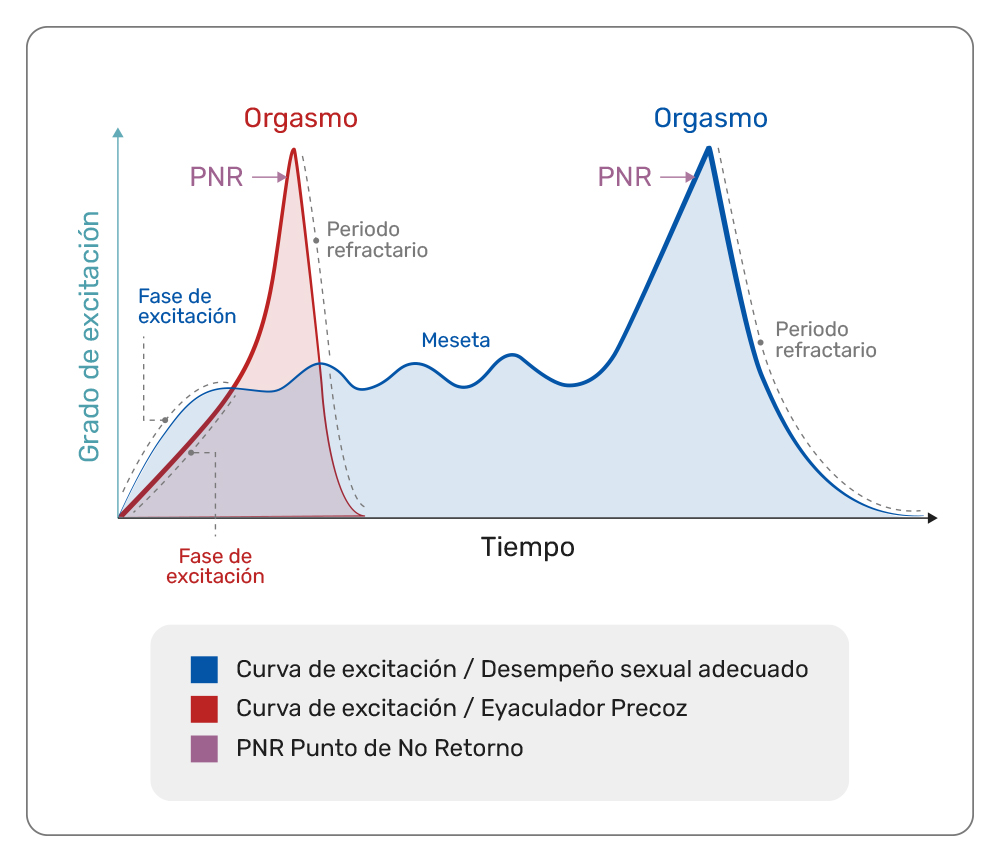
In lifelong premature ejaculation, which begins with a person's first sexual experience and continues over time, climax typically occurs within one minute. In acquired premature ejaculation, which develops after a period without ejaculation concerns, it usually happens within three minutes.
Notably, this definition focuses on heterosexual vaginal sex. There is limited information on how to define premature ejaculation in the context of anal sex or same-sex encounters.
Since PE is often self-reported and diagnosed based on distress rather than clear medical signs, its true prevalence is hard to measure. Older studies reported that 20–30% of men experienced PE. However, newer research using stricter criteria suggests the actual rate is closer to 5%.
What causes premature ejaculation?
he exact causes of premature ejaculation aren’t fully understood.
Yet for lifelong PE, experts believe it’s mainly due to changes in brain chemicals that help regulate ejaculation. Increased sensitivity of the penis head, erectile difficulties, genetic differences, hormone imbalances, and prostate problems may also play a role.
On the other hand, acquired PE is usually linked to medical, mental health, or relationship issues.
Common premature ejaculation treatments
Topical anesthetics, including numbing or desensitizing gels, creams, and sprays, are commonly used as a premature ejaculation treatment. (Pictured above: Kiiroo's Delay Gel)
Since the 1990s, premature ejaculation has mainly been treated with topical anesthetics, antidepressants, and behavioral therapy. While they may offer temporary relief for some, PE often returns once they're discontinued.
Topical anesthetics such as numbing creams or sprays used before sex are not popular. Up to 75% of men report dissatisfaction, and only about 10% keep using them.
Selective serotonin reuptake inhibitors (SSRIs) may delay ejaculation by boosting serotonin, but many men stop due to minimal effects.
As for behavioral therapy, it teaches techniques to build confidence and reduce anxiety during sex. It helps 45–65% of men in the short term, though long-term effects are still uncertain.

Masturbation aid devices
Research suggests masturbation aids that incorporate behavioral therapy, such as the Happy Pi Endurance Trainer, could be a viable premature ejaculation treatment.
Beyond nerve stimulation, researchers have also explored physical tools to help retrain arousal response. One approach pairs behavioral training with the Happy Pi device, a masturbation aid designed to reduce sensitivity and simulate intercourse.
In a clinical trial, 52 men completed an eight-week sphincter control program; half used the Happy Pi device alongside the training.
Though only 40 participants completed the study, those who used the device lasted about 90 seconds longer during sex. In comparison, the group that did training alone improved by just 30 seconds.
The findings suggest the device may enhance behavioral training by offering more targeted stimulation.
.jpg)
Advancing treatment for premature ejaculation
Premature ejaculation has long lacked reliable, long-term solutions, but early research into emerging technologies offers promise.
From nerve stimulation patches to smart training devices, these innovations have shown meaningful gains in ejaculation time with minimal side effects. Noninvasive and drug-free, they could mark a shift toward more flexible, on-demand treatment options—making spontaneous sex more feasible than with creams or pills that require advance use.
Still, larger and longer-term studies are needed to confirm their effectiveness. Future research should also explore how PE plays out in same-sex relationships, anal sex, and casual or newer partnerships.
For a condition that affects confidence, connection, and pleasure, innovation isn't just welcome—it’s overdue.
#sex doll #sex toys #sex toys for men #sex toys for female #sex toys for lesbian #dildos #vibrator #Masturbation #sex toys for women #sex toys for male #sex toys box #penis #vagina #Clitoral stimulation #anal toys #anal sex #climax #blow job #ejaculation#happypi#happypitech
